- About
- Solutions
Services
Solutions
- RCM Platform
- Case Studies
- Contact Us
- Blogs
Blogs
Enhancing the Abilities of Healthcare SectorServices
Solutions
RCM analytics is a dynamic solution designed to analyze, track, and optimize your revenue cycle management, which provides valuable insights for healthcare providers. OSP’s RCM analytics solution is equipped to enhance cash flow, reduce costs, and show areas for improvement within the revenue cycle. Our solution provides comprehensive metrics for tracking, such as denial rates, collection rates, and accounts receivable. Through this solution, we help uncover trends in payer performance, enabling strategic steps for improved cash flow and contract negotiations. Moreover, our system leverages predictive capabilities, foreseeing potential issues and allowing providers to address them proactively. With our expert team, we offer a tailored RCM analytics solution that meets the specific needs of healthcare organizations.
In OSP’s RCM analytics solution, AR Cycle Intelligence is fundamental for streamlining and optimizing account receivables. By leveraging analytics, we enable healthcare providers to identify bottlenecks, streamline AR workflows, and reduce the number of days. We offer a comprehensive view of the AR cycle through our analytics solution.
With AR cycle intelligence, we also help providers gain actionable insights into crucial metrics such as denials, reimbursement rates, aging of accounts, and more. These insights allow them to take prompt action against critical issues, resolve them, and accelerate reimbursement processes. We assure you that AR cycle intelligence in RCM analytics will empower providers. It will accelerate cash flow, reduce revenue leakage, and improve financial health.
Predictive Analytics is pivotal in the revenue cycle management system, as it offers financial forecasts to providers. Our analytics solution for the revenue cycle incorporates predictive analytics to anticipate upcoming financial and operational trends using algorithms and historical data. Using predictive analytics, we empower healthcare organizations to resolve their challenges.
Further, OSP’s RCM solution with predictive analytics helps providers identify and analyze patterns in claim denials and billing processes. Our solution also enables providers to make informed decisions using these insights. Besides, predictive analytics in our solution allows providers to anticipate patients’ behavior, facilitating the development of specific engagement and financial counseling strategies.
In the RCM solution, using analytics for payer denials mitigates challenges related to claim denials. OSP’s RCM analytics solution includes payer denial insights to address and resolve denial-related challenges. Moreover, payer denial insights in our RCM analytics solution aim to provide clinical staff with the reason behind denials. These insights also help them take correct measures to mitigate these denials.
Payer denial insights also help providers identify patterns and trends in denial data. Analyzing this data will enable them to reduce denial rates, optimize claim accuracy, and improve overall revenue capture. Further, these insights from analyzing payer denial data would allow providers to develop strategies for improving relations with payers and streamlining the reimbursement process. Above all, payer denial insights help healthcare organizations foster healthy collaborations with insurance companies and enhance financial health.
Performance management is a crucial aspect of RCM solutions. In our RCM analytics, performance management insights are essential in optimizing overall operational and financial performance. These insights offer a comprehensive view of KPIs across the healthcare organization’s revenue cycle. Through these KPIs, providers can monitor, assess, and improve the various aspects of financial processes.
Further, performance management insights enable providers to make data-driven decisions. Providers can leverage these insights to improve claims processing, reimbursement rates, and denial rates. It also facilitates the implementation of specific strategies that will reduce costs and improve revenue capture. Overall, performance management insights help providers improve efficiency and continuously ensure profitability.
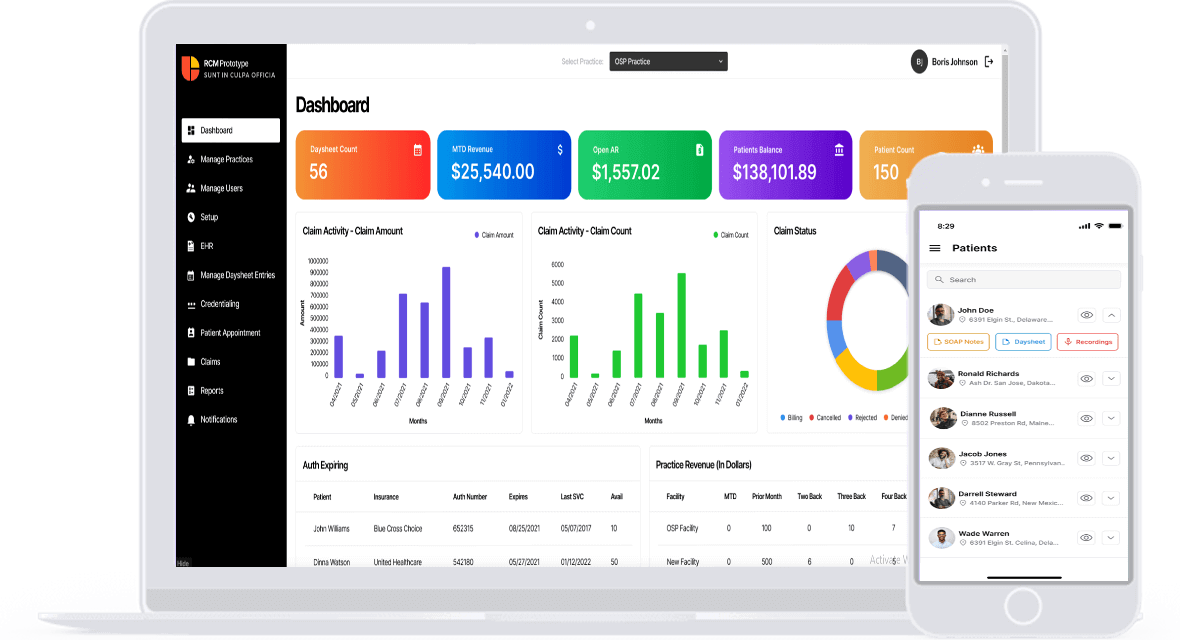
An intuitive scorecard dashboard is a powerful tool for viewing performance metrics. OSP’s RCM analytics include the scorecard dashboard that offers real-time snapshots of the healthcare organization’s financial health and operational efficiency. It also enables providers to assess and respond to revenue cycle processes seamlessly.
This dashboard also consolidates performance indicators in a user-friendly interface, such as claim processing times, reimbursement trends, denial rates, etc. Further, this dashboard helps providers monitor progress, point out areas of concern, and identify trends. Providers can leverage this scorecard dashboard to facilitate decision-making that will optimize workflows and improve the revenue cycle.
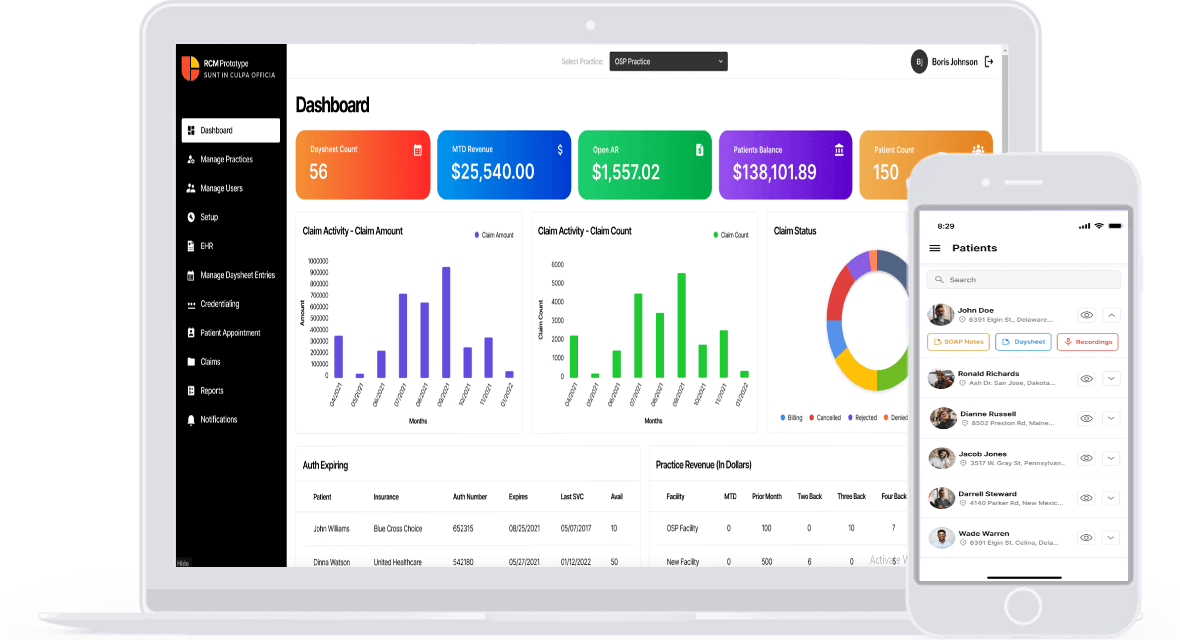
Our revenue cycle management system manages clinical records and handles insurance eligibility information, ledgers, patient demographics, emergency contacts, billing data, and other forms. This platform provides easy access to comprehensive patient data from a single location and integrates seamlessly with EHR and EMR systems. This integration saves time for healthcare providers by allowing them to concentrate on providing high-quality care rather than manually entering data. It is essential to keep accurate medical records to reduce human errors.
Learn more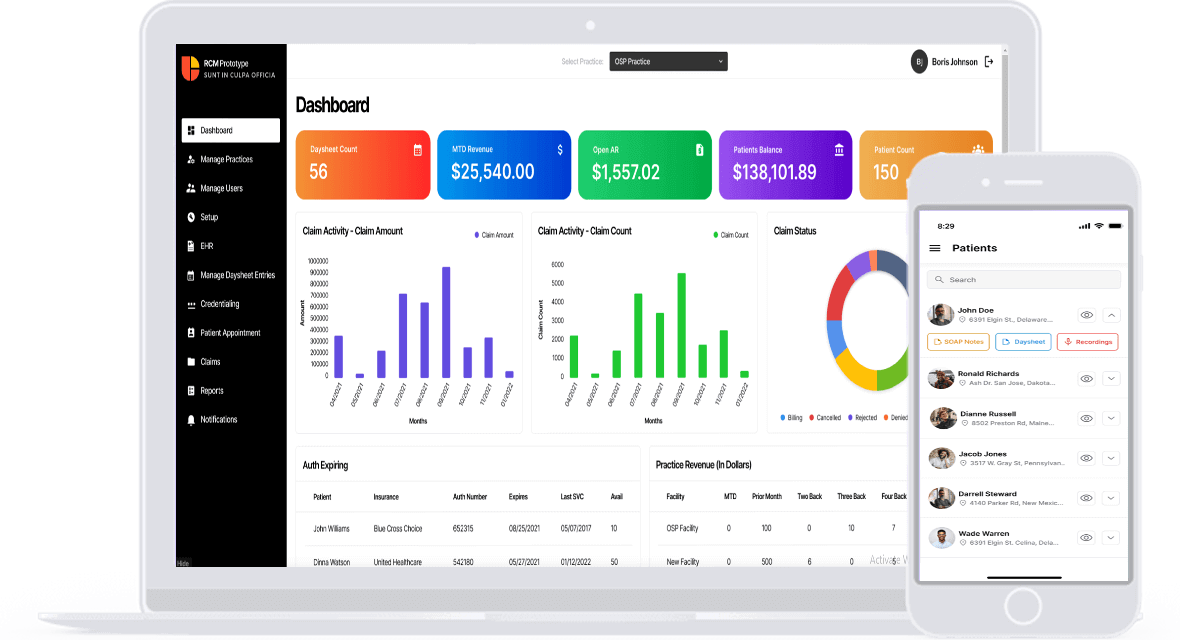
Revenue cycle management systems streamline medical professionals’ records by integrating provider data management and granting access to personal and business data. By providing direct access to, evaluating, and managing healthcare provider data, this integrated platform efficiently addresses instances of practitioner malpractice. Licenses and certificates are just a few of the numerous documents it effectively manages. Provider data management enhances healthcare revenue and helps insurance companies and practices monitor provider eligibility.
Learn more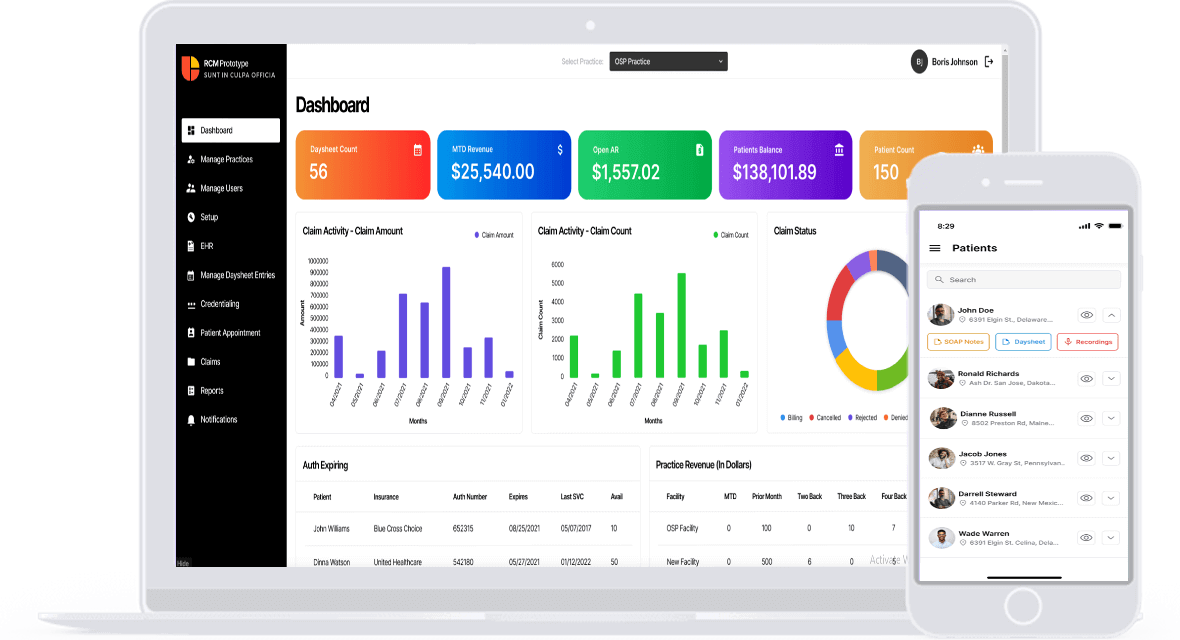
We have robust master data management features in our practice management RCM software. It also involves maintaining CPT codes and detailed fee schedules to ensure accuracy and remove errors. Other critical components managed by the healthcare revenue cycle system include ICD, place of service, taxonomy, facility, insurance, and submitter data. When correct bills with the right coding are submitted, denials decrease, wait times reduce, and revenue production increases.
Learn more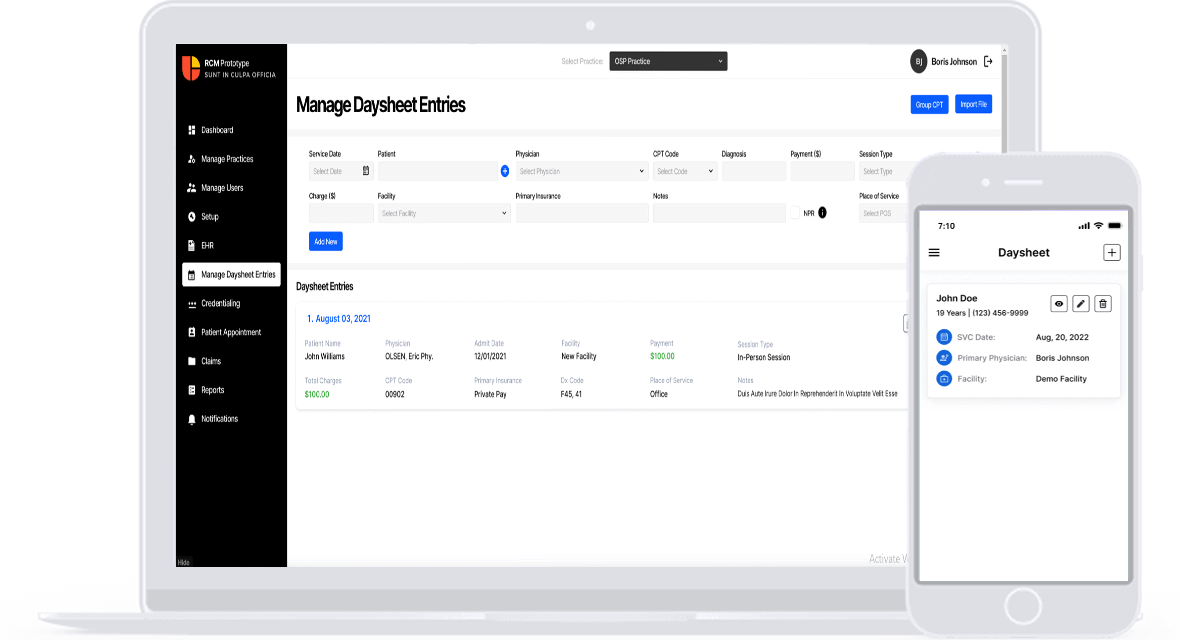
A healthcare revenue management platform that integrates medical sheet management ensures revenue optimization, compliance adherence, and accurate billing. This feature gives you daily summaries of patient encounters, making it easier to track and record billable services. Coding errors, missed charges, and denied claims are all reduced. This feature financially helps healthcare practices while increasing practice productivity and revenue collection.
Learn more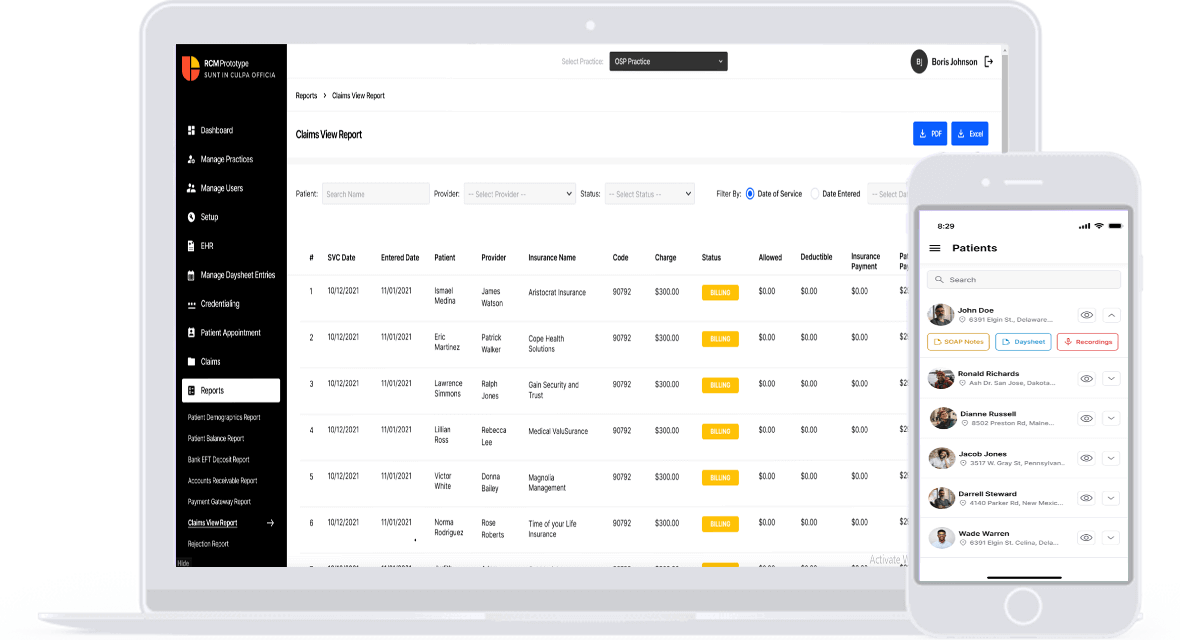
With its features for processing and submitting claims, revenue cycle management software helps providers submit them accurately and quickly. Its support for paper claims in HC1500 format and electronic claims in 837 format allows for the facilitation of traditional and modern workflows. Healthcare practitioners can submit accurate claims quickly and efficiently thanks to this flexibility. Ultimately, maximizing revenue and maintaining stable finances are the results of timely claim submission.
Learn more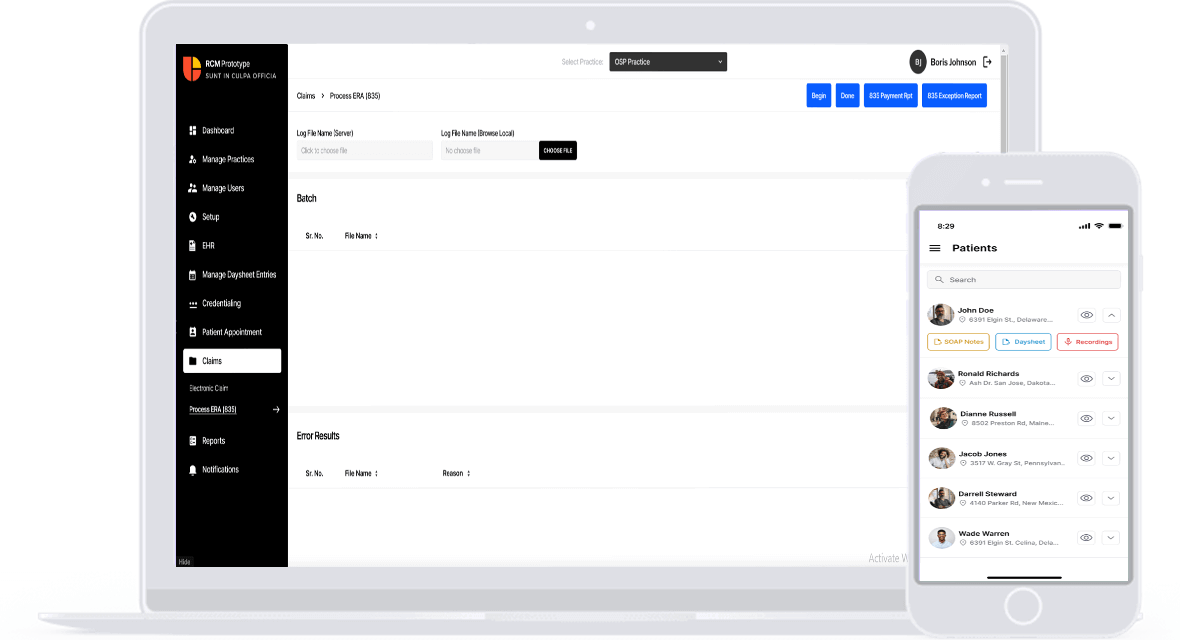
Advanced revenue cycle management software uses a powerful claims rule engine to decrease denial rates and enhance claims processing. The software can process claims more quickly and accurately, reducing errors and expediting reimbursement, thanks to the engine’s management of claim rule components.
Learn more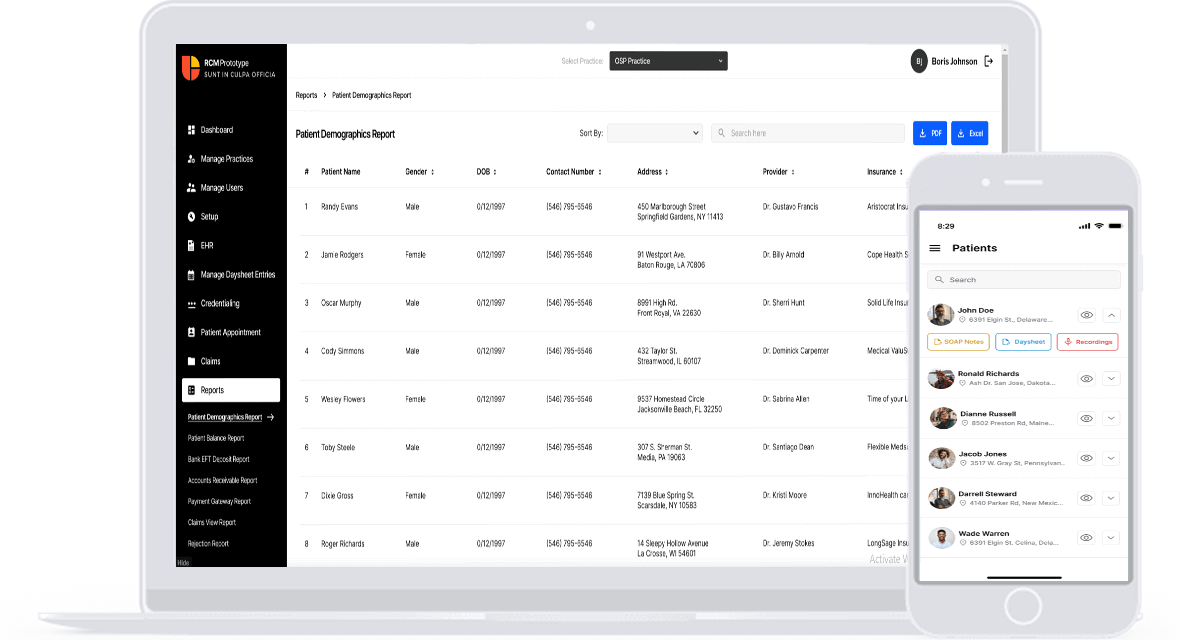
One of the most important functions of hospital revenue cycle management systems is confirming insurance eligibility. Through the verification of patients’ insurance benefits and coverage, this innovative feature streamlines the revenue cycle. Automated verification of insurance eligibility guarantees precise patient obligations and minimizes claim rejections due to eligibility problems. By informing patients of their financial responsibilities for their medical care, the RCM platform’s integration of this verification improves patient education and revenue predictability.
Learn more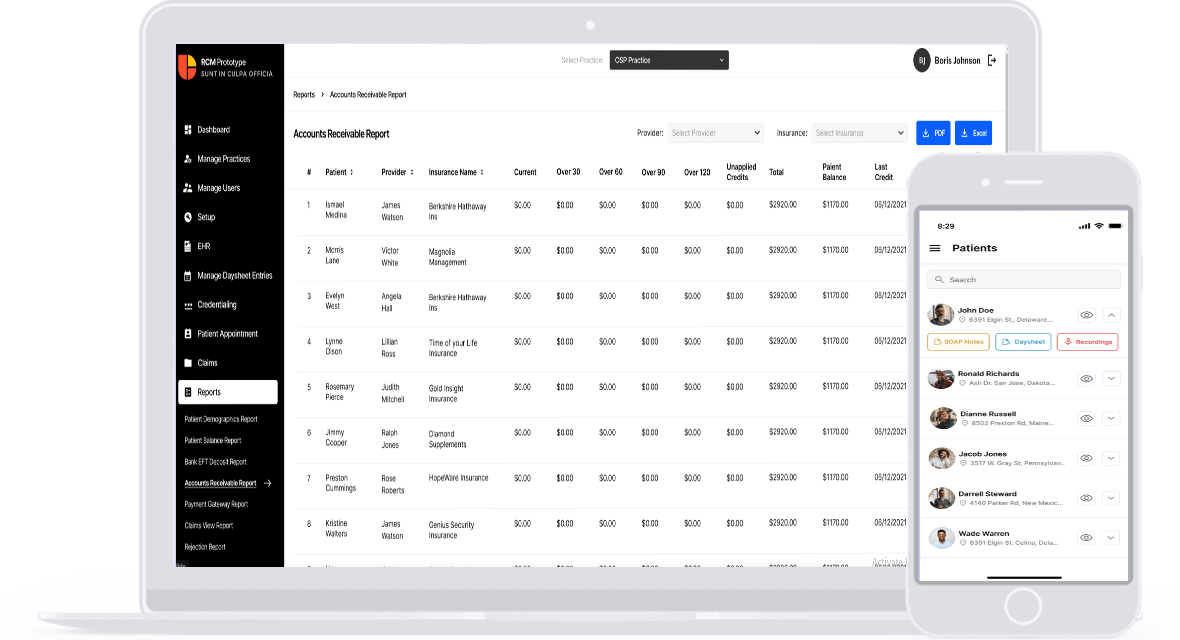
To help practitioners optimize their revenue cycle, we developed revenue cycle management with A/R management in mind. This feature makes more effective administration of patient balances and unpaid claims possible. It offers resources for tracking, evaluating, and pursuing outstanding claims, decreasing A/R aging, and speeding up cash flow. This feature also makes billing easier by detecting and minimizing revenue leakage and improving financial performance.
Learn more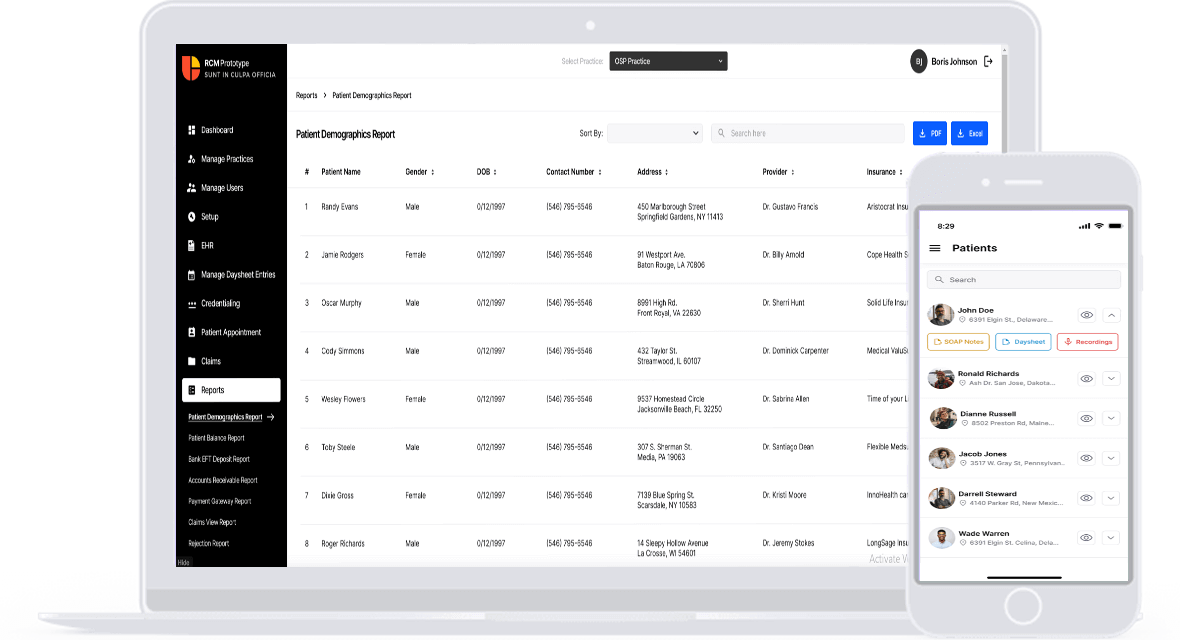
Prior authorization is a fundamental component of the RCM system that we designed. It expedites the drawn-out process of getting approval for surgeries and medical treatments. RCM software optimizes and automates processes to reduce administrative work, improve care coordination, and guarantee prompt intervention for critical treatments. Above all, this RCM system function increases healthcare providers’ revenue and decreases rejected claims.
Learn moreOur solution employs advanced analytics to pinpoint revenue leakage sources, such as under-coding, unpaid claims, or inefficient collection practices. This analysis guides corrective actions, empowering healthcare providers to recover lost income and optimize revenue streams effectively. Our custom RCM solution allows practitioners to seamlessly integrate this powerful tool into their operations, ensuring enhanced financial performance and operational efficiency.
Our solution leverages descriptive and diagnostic analytics to identify inefficiencies in the revenue cycle, claim denials, or delayed payments. Healthcare providers can streamline operations by addressing these issues, fostering a quicker and more efficient revenue cycle. Our custom RCM solution ensures providers gain a comprehensive tool to enhance operational efficiency, leading to improved financial performance and a smoother workflow in healthcare management.
Using analytics to study patient behavior allows healthcare providers to personalize communication and enhance service delivery. For instance, predictive analytics can identify patients likely to face challenges in paying their bills. It also enables a proactive approach with tailored payment plans or financial counseling. We offer customizable solutions to meet the specific needs of healthcare providers, ensuring improved operational performance and patient satisfaction.
In a robust RCM analytics system, crucial components include patient registration, appointment scheduling, charge capture, coding, claims submission, payment processing, data analytics, data quality validation, data integration and management, choosing the right tools, contract and payer analytics, and comprehensive data management. These components ensure accurate billing, streamlined operations, and enhanced patient experiences throughout the RCM process, optimizing financial performance and supporting data-driven decision-making.
Optimize revenue management in healthcare by seamlessly integrating RCM analytics with EHR systems and financial software. This ensures efficient data flow, providing actionable insights into patient financials, claims denial rates, and revenue cycle processes. Automation tools capture charges for virtual visits, enhancing efficiency and enabling real-time financial reporting. This integration transforms data into robust plans, improving workflow efficiency, reducing costs, and enhancing patient satisfaction and revenue management.
Common data standards and formats in RCM analytics include HL7, ensuring interoperability in health data exchange; X12 for electronic data interchange (EDI) in financial transactions; and ICD-10, a diagnostic coding system for medical billing. These standards provide a structured framework, ensuring consistency and interoperability in organizing and exchanging financial and billing data. They streamline data exchange, improve accuracy, and enhance stakeholder interoperability in revenue cycle management.
Healthcare organizations safeguard sensitive patient and financial data during RCM analytics through crucial measures. Robust data encryption prevents unauthorized access, while role-based access control ensures limited access. Adherence to regulations, especially HIPAA, ensures ethical practices. Regular internal audits identify vulnerabilities and ensure compliance. Ongoing staff training promotes data security awareness. Robust data governance protocols maintain integrity and security throughout the RCM process, fostering trust in data handling practices.
Healthcare organizations uphold data accuracy and consistency in RCM analytics across diverse facilities. Emphasizing data quality and validation with governance protocols ensures accuracy. Standardizing data using HL7, X12, and ICD-10 promotes consistency. Automated data management streamlines access, normalization, and validation. Role-based access control ensures security and compliance. Ongoing staff training and robust governance fortify data integrity and security throughout the RCM process.
Healthcare organizations employ strategic technical approaches for automated financial data collection in RCM analytics. Robotic Process Automation (RPA) reduces errors in tasks like data entry, enhancing efficiency. Integration with EHR/EMR and Practice Management Systems ensures streamlined data exchange and billing consistency. Advanced data analytics, driven by artificial intelligence, yields actionable insights into revenue trends. Real-time monitoring and reporting of claims system metrics offers valuable insights. Comprehensive data management automates capture, normalization, and validation, enhancing revenue management.
By adopting strategic measures, healthcare organizations can ensure their RCM analytics align with evolving regulatory demands. Continuous monitoring of healthcare regulations, coding standards, and reimbursement models is vital for staying abreast of changes and ensuring ongoing compliance. Implementing agile RCM systems facilitates easy adaptation to evolving regulatory requirements, ensuring sustained compliance. Leveraging data analytics enables organizations to monitor and adapt RCM processes to meet evolving regulations. At the same time, integration with regulatory updates and collaboration with experts ensures prompt adjustments to remain compliant with changing requirements.
Ensuring accurate financial data for revenue forecasting in RCM analytics involves robust practices. Healthcare organizations implement data validation processes, assessing completeness, consistency, correctness, and reliability. Automation of data capture and normalization enhances accuracy by standardizing data. Data governance protocols ensure integrity, quality, and security, contributing to reliable decision-making. Leveraging advanced analytics identifies trends, facilitating informed decisions. Continuous monitoring and review provide accuracy, prompt adjustments, and sustained data quality.
To ensure patient privacy and comply with regulations like HIPAA in RCM analytics, healthcare organizations implement crucial measures. For e.g., robust data encryption shields sensitive patient and financial data from unauthorized access. Role-based access control limits data access to authorized personnel, minimizing the risk of misuse. Adherence to healthcare regulations, including HIPAA, and regular internal audits ensure security and compliance. Ongoing staff training and robust data governance protocols bolster patient data integrity and security throughout the RCM process.
Adapting RCM analytics to evolving billing and coding standards involves strategic measures. Advanced data analytics, powered by artificial intelligence, provides actionable insights into revenue trends and coding standards. Seamless integration with EHR systems ensures comprehensive data capture, aligning with the evolving healthcare landscape. Continuous monitoring of regulatory updates and implementing agile RCM systems enable healthcare organizations to comply with evolving billing and coding standards.
Healthcare organizations utilize RCM analytics to identify and address the root causes of claim denials. These analytics provide data-driven insights into denial patterns and causes, enabling providers to develop targeted strategies for reducing denials and optimizing revenue cycle performance. Predictive analytics proactively identify common reasons for denials, allowing refinements to front-end processes. Comprehensive data management through RCM analytics offers diagnostic and root cause analyses, empowering providers to tailor appeals with supporting documentation for specific denial reasons.
Healthcare organizations strategically leverage technology and data analytics to optimize Revenue Cycle Management in Value-Based Care, enhancing financial performance and patient satisfaction. Embracing data-driven approaches ensures sustained value from RCM investments, with real-time insights and advanced analytics automating analysis for informed decision-making. Increasing IT investments underscore the industry’s recognition of technology’s importance in optimizing financial and operational efficiency, as reflected in the growing global Healthcare Revenue Cycle Management market.